General Effects: Clinical Case Study
General Effects of Neurological Dysfunction |
HPI: You are on-call in the intensive care unit one night and are called to the bedside of BD, a 19-year-old male who was in a motorcycle accident 3 nights ago. He was riding his motorcycle without a helmet and struck a meridian. He flew off the motorcycle approximately 30 feet before striking the side of a truck. He sustained significant head injuries and has yet to regain consciousness. You are called, as the nurse noticed his body position was changing. P/E: He remains in a coma and has remained intubated and mechanically ventilated since admission to hospital. His vitals have been fluctuating somewhat. Current vitals: HR 96; RR (vent) 16; BP 140/97 mm Hg; afebrile; SaO2 94%. BD is lying supine with his lower limbs fully extended and his feet fully plantar flexed. His arms are now held in flexion at the elbows and wrists (see Figures 1 and 2). He provides no response (eye opening, verbal, or motor) to either verbal commands or painful stimuli. |
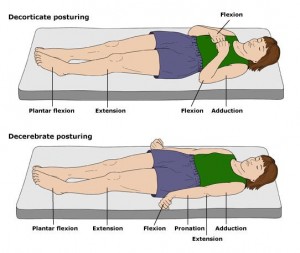
Figure 1 |
| Question | Your Answer |
What is the most likely diagnosis? |
Severe traumatic brain injury |
Contrast the two types of posturing associated with this condition. |
Decorticate posturing involves flexion of the arms, wrists, and fingers, along with extension of the lower extremities. It is associated with severe damage to the cerebral hemispheres (see Figure 1). Decerebrate posturing involves extension of both the upper and lower extremities and is associated with brain stem lesions (see Figure 2). |
If this patient were able to recover to the point where he opened his eyes to pain, localized motor responses to pain, and spoke inappropriate words, what would his Glasgow Coma Scale score be? |
Eyes: 2 Total: 10 |
Is there anything in the mother’s history that might have predisposed her to having a child with this condition? |
There is some research that suggests a deficiency of folate, a risk in vegetarian diets, may be associated with spina bifida. For this reason, all women in child bearing years are encouraged to take folate supplements, before becoming pregnant. |
How can understanding whether upper or lower motor neurons are injured help you localize the damage? |
Damage to upper motor neurons (in the corticospinal tracts and the posterior zone of the frontal cortex) causes weakness or paralysis on the contralateral side of the body. Damage to lower motor neurons (in the anterior horn cells of the spinal column and the brainstem (cranial nerves) causes weakness or paralysis on the ipsilateral (same)side of the body. |
What are the criteria used to define “brain death”? |
1) Cessation of brain function (flat/inactive EEG); |
What is the difference between Broca’s aphasia and Wernicke’s aphasia? |
Broca’s area (dominant frontal lobe, inferior motor cortex) is involved in motor actions required for logical speech. Damage to this area results in a motor or expressive aphasia, where patients construct appropriate words or responses. Wernicke’s area (left temporal lobe) is involved in processing sensory information (i.e., making sense of things). Damage to this area results in a receptive or sensory aphasia, where the patient is unable to understand written or spoken words. |
If, when you assessed this patient’s eyes, you found a “blown pupil,” what would this indicate? |
A unilateral dilate pupil that is unresponsive to light is an indication of intracranial herniation where increased intracranial pressure has pushed a portion of the brain into an adjoining area. |
Why should you never perform a lumbar puncture on a patient with significant brain trauma? |
The cerebral inflammation and edema that accompanies brain trauma increases intracranial pressure. If this is significant, the introduction of a needle into the CSF space in the lower spine will create a release of pressure at that point, allowing the intracranial pressure to push the midbrain and diecephalon into the foramen magnum (transtentorial herniation). |