Congenital Neurological Disorders: Clinical Case Study
Congenital Neurological & Disorders Seizures |
|
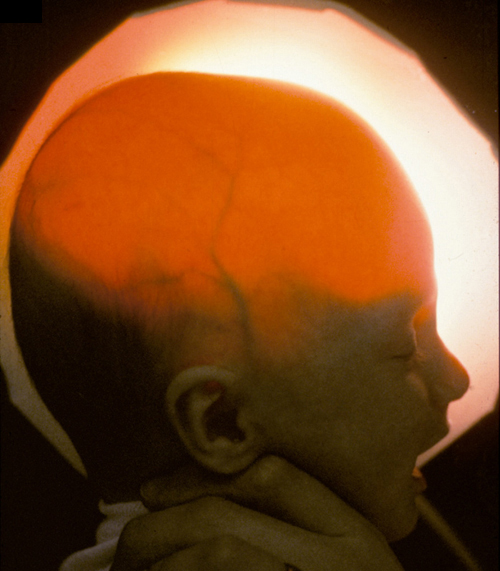
HPI: You are called to the delivery suite at the local hospital to evaluate a newborn male child with an enlarged head. The obstetrician delivered the child via cessation section due to enlarged head size on ultrasound. The delivery by C-section was uncomplicated but the infant was born with flaccid lower extremities and a mass on his lower back. PMI: The infant’s mother avoided contact with doctors until 32 weeks gestation, at which time an ultrasound identified the enlarged head. The infant’s mother was healthy, athletic, and adhered to a strict vegetarian diet. P/E: The infant boy is lying in the warmer with arms flexed and legs extended. The infants head measures 46 cm. (normal 32–38.5 cms). Shining a light against the scalp reveals transillumination (see Figure 1). Pupils are equal and reactive, but the sclera (white portion of the eyes) superior to the pupils can be seen. The scalp is fluctuant and the cranial sutures are widely displaced. Cardiorespiratory and abdominal exams are unremarkable. Neurologic examination reveals flaccid paralysis of the lower extremities bilaterally with absent reflexes. Upper extremity examination is normal. Examination of the back reveals a mass in the midline that does not transilluminate (see Figure 2). |
|
| Question | Your Answer |
What is the most likely diagnosis? |
Spina bifida |
What are the 3 types of this condition, how do they differ, and which is likely in this case? |
Spina bifida occulta: incomplete fusion of the spinous processes, without herniation of meninges or neural tissue Meningocele: Same as above but with protrusion of the meninges through the spinal defect. These masses will transilluminate. Meningomyelocele: Same as above, but with herniation of both the spinal cord and meninges through the defect. This is often associated with neurological disabilities. As these masses are full of tissue, they will not transilluminate. This is the most likely diagnosis in this case. |
What tests might have been done earlier in the pregnancy that might have detected this condition earlier? |
Alpha-fetoprotein leaks from the defect and causes an elevation in maternal blood first detectable from 16–18 weeks gestation. This can also be detected in the amniotic fluid by amniocentesis. |
Is there anything in the mother’s history that might have predisposed her to having a child with this condition? |
There is some research that suggests a deficiency of folate, a risk in vegetarian diets, may be associated with spina bifida. For this reason, all women in child bearing years are encouraged to take folate supplements, before becoming pregnant. |
Why can early detection of this condition be helpful? |
In addition to ensuring adequate preparation for delivery, some cases have been operated on in utero with success. |
Why is a careful examination of the infant girl important? |
With meningomyeloceles there is involvement of the spinal cord and neurological complications are common. A careful examination is important to identify any neurological concerns, including difficulty voiding, that left untreated could result in further complications. |
What malformation is likely the cause of the increased intracranial CSF? |
Most infants born with meningomyeloceles have type II Arnold-Chiari malformations. Arnold-Chiari malformation are abnormalities at the medullary-spinal junction. Type I (usually diagnosed in adulthood) involves the cerebellar tonsils lying below the level of the foramen magnum. Most are asymptomatic. Type II Arnold-Chiari malformations involve the cerebellar vermis, medulla, and the fourth ventricle lying below the level of the foramen magnum. This leads to obstructive hydrocephalus, as evidenced in this case. |