Congenital Heart Disease: Clinical Case Study
Congenital Heart Defect Case |
HPI: You are called to the newborn nursery to assess HP, a 2-day-old infant male with poor feeding. The child has lost weight since birth. PMI: HP was the product of an unremarkable 39-week first pregnancy of a 28-year-old mother and 31-year-old father. Labor was slightly prolonged but otherwise unremarkable, and HP was born by spontaneous vaginal delivery. Birth weight was 8 lbs 6 oz (3,850 gms). There were no concerns and the child began breastfeeding within the first 30 minutes. Feedings were normal until yesterday, when HP seemed to tire quickly after starting to feed. P/E: Pale infant in mild-moderate respiratory distress. Vitals: HR 110; RR 28; BP 85/65; Temp 37.2°C (99°F); Wt 7 lbs 6 oz (3,400 gms). Examination of the infant’s chest reveals a hyperdynamic precordium, with a palpable thrill over the mid-sternum area. A loud halosystolic murmur is heard in the left lower sternal border. Crackles are heard through the lower lung fields bilaterally. Peripheral pulses are decreased Investigation: Chest X-ray reveals an enlarged heart and evidence of interstitial fluid in the lungs (see Figure 1). |
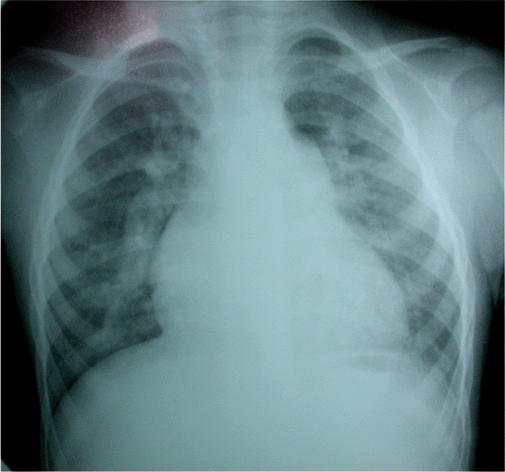
Figure 1. Chest X-ray showing increased pulmoinary and arterial vasculature. When the right atrium and left ventricle are enlarged, a communication between chambers must be considered. |
| Question | Your Answer |
What is the most likely diagnosis? |
Large ventricular septal defect (VSD) |
Why is the child having difficulty feeding? |
The large VSD pushes blood from the high pressure left ventricle through to the lower pressure right ventricle. This means a larger amount of blood goes to the lungs (some already oxygenated) and a smaller amount to the brain and body, resulting in decreased oxygen delivery to tissues. When the baby feeds (a strenuous activity for an infant), he quickly tires. |
Why is this baby not cyanotic? |
While a smaller amount of blood is going to the body than would normally be the case, that blood is well oxygenated. Cyanosis only occurs when a significant amount of the blood is unoxygenated. |
If left unchecked, what complication might occur that might turn the infant cyanotic? |
If the high blood flow to the lungs persists, the muscular layer of the blood vessels in the lungs may build up, irreversibly increasing the right-sided pressure (pulmonary hypertension). Eventually, this pressure may become higher than left sided pressures, and the flow through the VSD would reverse. In that case, some of the unoxygenated blood in the right ventricle bound for the lungs would be shunted across to the left side. This reversal of flow is called Eisenmenger’s Syndrome. |
What are the four components of Tetralogy of Fallot? |
|
Is Tetralogy of Fallot considered a cyanotic congenital heart defect, and, if so, why? |
TOF is a cyanotic congenital heart condition because the stenosis of the pulmonary valve increases the pressure in the right ventricle. If this pressure is greater than that in the left ventricle, unoxygenated blood would flow to the periphery and cause the appearance of cyanosis. These are commonly called “Tet spells” and are often relieved by squatting. |